What is degenerative disc disease?
Degenerative disc disease (DDD) is a condition that affects the intervertebral discs in the spine. Discs act as cushions between the vertebrae, providing support, flexibility, and shock absorption. Over time, the discs can degenerate or break down, leading to degenerative disc disease. The degeneration typically occurs as a natural part of the aging process but can also be accelerated by factors such as genetics, lifestyle choices, and injury.
The prevalence and impact of degenerative disc disease
The impact of degenerative disc disease can vary depending on the severity of the condition and individual factors. Degenerative disc disease may be asymptomatic and not cause any significant problems. However, when symptoms do occur, they can have a significant impact on a person’s quality of life.
Understanding degenerative disc disease
The exact cause of DDD is not always clear, but it generally develops over time due to a combination of factors. Factors include:
- Aging: Intervertebral discs naturally undergo wear and tear. The discs lose some of their water content, become less flexible, and may develop small cracks or tears.
- Genetics: Some may inherit genes that make their discs more susceptible to degeneration or less capable of repairing themselves effectively.
- Spinal injuries: Accidents, falls, or repetitive activities that strain the spine can lead to disc damage and accelerate the degenerative process.
- Poor posture and body mechanics: Poor posture, such as slouching or frequently bending and twisting the spine improperly, can put excessive stress on the intervertebral discs and contribute to disc degeneration.
- Overweight or obesity: Carrying excess weight puts additional strain on the spine.
- Smoking: Smoking may impair the blood supply to the discs, affecting their nutrition and ability to heal.
- Sedentary lifestyle: Lack of regular physical activity can weaken the muscles that support the spine.
If you suspect you have degenerative disc disease or are experiencing symptoms related to your spine, please consult a healthcare professional for an accurate diagnosis and appropriate treatment options. Locate a surgeon near you today.
Symptoms and diagnosis
DDD typically occurs with age, and it can cause a variety of symptoms. Here are some common symptoms associated with degenerative disc disease:
- Back pain: Persistent or recurring pain in the lower back may be dull or sharp and can range from mild to severe. It is usually exacerbated by activities such as bending, lifting, or twisting.
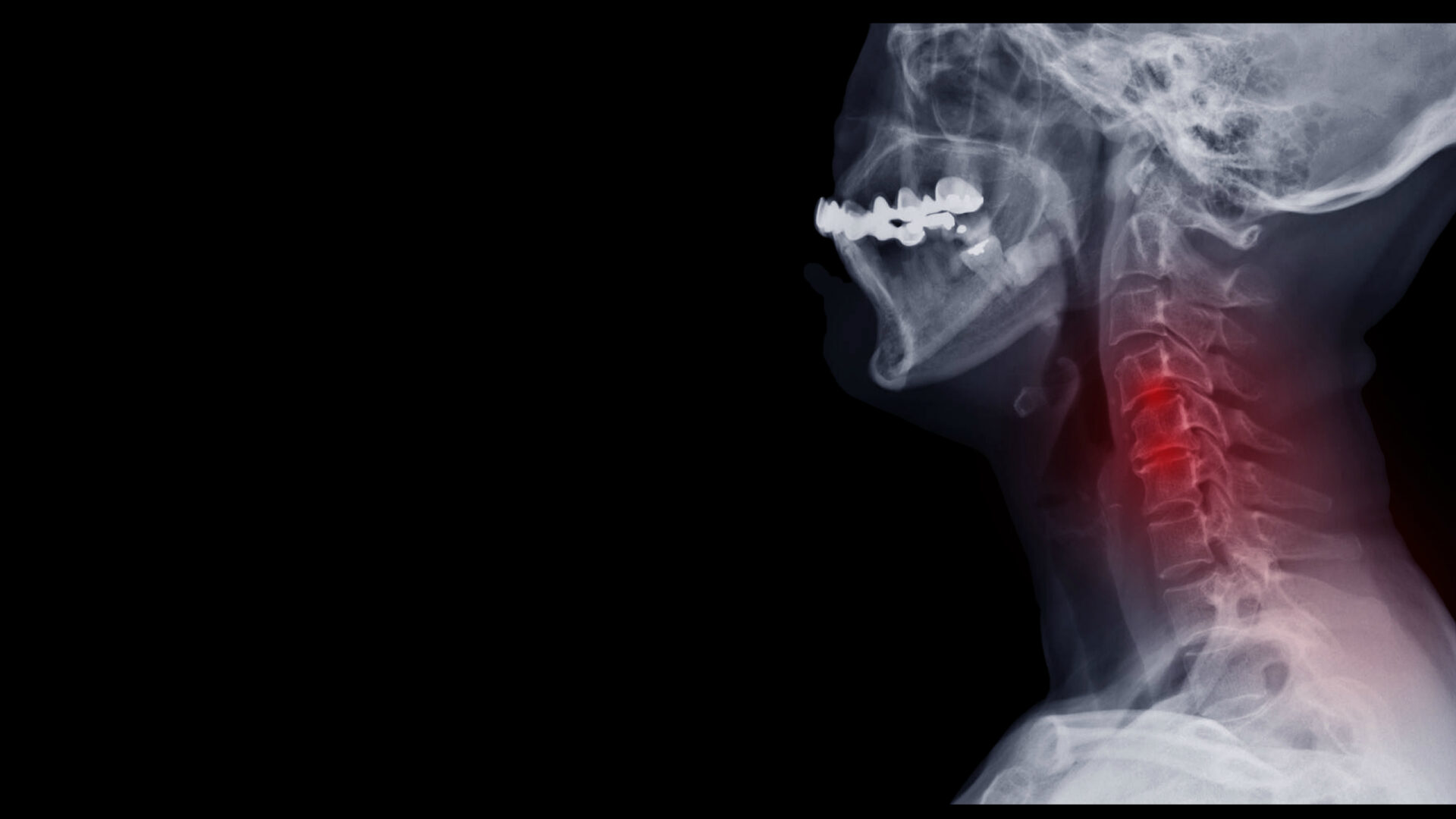
- Neck pain: DDD can also affect the cervical spine, leading to neck pain. The pain may radiate to the shoulders, upper back, and arms.
- Pain that worsens with movement: Activities that put pressure on the affected discs, such as lifting, sitting, or standing for prolonged periods, can intensify the pain.
- Stiffness: People with DDD may experience stiffness in the spine, making it difficult to bend or twist.
- Numbness and tingling: When degenerated discs press against spinal nerves, it can cause numbness, tingling, or a pins-and-needles sensation. These symptoms can radiate to the arms, hands, legs, or feet, depending on the location of the affected discs.
- Weakness: DDD may lead to weakness in the muscles served by the affected nerves. This can cause difficulty in gripping objects, lifting, or performing fine motor skills.
- Changes in posture: As DDD progresses, individuals may exhibit changes in their posture. They may develop a stooped or hunched posture, or they may lean to one side to relieve the pain.
- Limited mobility: The pain and stiffness associated with DDD can restrict the range of motion in the spine, making it difficult to perform certain movements.
It’s important to note that not everyone with degenerative disc disease experiences symptoms, and the severity and combination of symptoms can vary from person to person.
Diagnostic methods and procedures
It’s important to consult with a qualified healthcare professional for an accurate diagnosis and appropriate treatment plan. That being said, here are some common steps involved in diagnosing DDD:
- Medical History: Your doctor will address your symptoms and ask about any pain, numbness, tingling, or weakness you may be experiencing, as well as any previous injuries or conditions that could contribute to your symptoms.
- Physical Examination: A physical examination will assess your range of motion, reflexes, muscle strength, and any signs of nerve involvement.
- Imaging Tests: Various imaging tests can help confirm the diagnosis of DDD and assess the extent of the condition. These tests may include:
- X-rays: Can reveal changes in the structure of the spine, such as narrowing of the disc space, bone spurs, or misalignment.
- Magnetic Resonance Imaging (MRI): Uses magnetic fields and radio waves to produce detailed images of the spine. It can help visualize the discs, nerves, and surrounding structures, enabling your doctor to detect any degenerative changes or disc herniation.
- Computed Tomography (CT) Scan: Takes cross-sectional images of the spine and can provide detailed information about the bones and their alignment. This test may be used to assess the spinal canal and nerve roots.
- Discography: Involves the injection of a contrast dye into the affected disc(s) to evaluate their integrity and identify the source of pain.
The need for effective treatment options
While there is currently no cure for DDD, several treatment options aim to manage symptoms, improve function, and enhance the overall well-being of individuals with the condition. Treatment plans should be personalized based on an individual’s specific condition and symptoms.
Conventional treatments for degenerative disc disease
Below are some conventional treatments commonly used for degenerative disc disease:
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, can help reduce pain and inflammation associated with DDD. Short-term use of muscle relaxants or oral steroids may be prescribed to relieve acute symptoms.
- Physical therapy: Can provide exercises and stretches to strengthen the muscles supporting the spine and improve flexibility. May include techniques like heat or cold therapy, ultrasound, electrical stimulation, and traction to alleviate pain and promote healing.
- Pain management injections: Epidural steroid injections may relieve severe pain and inflammation. Injections deliver corticosteroids directly into the space around the affected nerve roots, providing temporary relief.
- Bracing: A back brace can provide support and stability to the spine, reducing pain and discomfort.
- Lifestyle modifications: Maintaining a healthy weight, practicing good posture, and avoiding activities that strain the spine can help manage symptoms and slow down the progression of DDD.
- Assistive devices: Lumbar supports, ergonomic chairs, or specially designed cushions can help reduce discomfort and provide better spinal alignment during daily activities.
- Alternative therapies: Complementary and alternative therapies, such as chiropractic care, acupuncture, massage therapy, or yoga may provide relief.
- Surgical interventions: Surgical options for DDD include discectomy (removal of the damaged disc), spinal fusion (joining vertebrae together to stabilize the spine), or artificial disc replacement (implanting an artificial disc).
- Epidural steroid injections: Corticosteroids are strong anti-inflammatory medications and, when placed into the epidural space, can significantly reduce inflammation around an irritated nerve that is causing back and leg pain and discomfort.
- Facet joint injections and nerve blocks: Facet joint injections and medial branch blocks aim to treat pain arising from facet joints in the spine. While facet joint injections are given directly into the facet joint, medial branch blocks target the medial branch nerves that carry pain signals from the facet joints to the brain.
Surgical options for degenerative disc disease
Surgical treatment for degenerative disc disease is typically considered when conservative treatments have not provided sufficient relief. Here are some surgical options that may be considered:
- Spinal Fusion: Aims to stabilize the affected spinal segment by fusing two or more vertebrae together. It involves removing the damaged disc and using bone grafts or implants to promote fusion and eliminate motion at the affected segment.
- Artificial Disc Replacement: The diseased disc is removed and replaced with an artificial disc. Artificial Disc Replacement aims to maintain motion at the affected segment while relieving pain and reducing the need for adjacent level degeneration that may occur after spinal fusion.
- Microdiscectomy: Typically used to treat DDD-related herniated discs. It involves removing the portion of the disc that is pressing on a nerve root or spinal cord, relieving pain and other associated symptoms.
- Laminectomy: Laminectomy involves removing a portion of the lamina (bony arch) of the affected vertebra to relieve pressure on the spinal cord or nerve roots.
- Intradiscal Procedures: Certain minimally invasive techniques, such as nucleoplasty or intradiscal electrothermal therapy (IDET), involve using heat or other methods to treat the affected disc directly.
The choice of surgical treatment depends on various factors, including the severity and location of disc disease, overall spinal health, and individual patient characteristics. Suitability should be assessed by a qualified healthcare professional after a thorough evaluation of the specific case. To find a physician, please use the following link. Locate a surgeon near you today.
Stay tuned for part 2-
In our next blog, we will continue our discussion on degenerative disc disease. Topics will include emerging treatments, lifestyle modifications, ways to cope with your diagnosis, assistive devices, and new areas of research in the area of degenerative disc disease.